What health coverage program options for uninsured children in North Dakota are available?
Who can apply for programs or services?
Generally speaking, anyone may apply for assistance. Eligible applicants will ordinarily reside in North Dakota.
Where do I apply for programs and services?
To apply, contact your local County Social Service Office. For local contact information, click on the county closest to your home on the locator map. You may also view the Application for Assistance, complete it, print and sign it, and deliver it to the County Social Service Office. Completing the application prior to visiting the County Social Service Office may help to shorten the eligibility determination process. You can also complete and file the application electronically using the online application system.
Will there be any cost to me for programs or services?
Some people are required to pay co-payments for services received, and some may also be required to pay a recipient liability. Individuals DO NOT have to pay co-payments if they:
· Are younger than age 21
· Are pregnant
· Are tribal members enrolled in Medicaid and receiving services under a referral from Contract Health Services (CHS)
· Need emergency services
· Receive family planning services
· Receive Medicaid through the Women's Way or Medicaid Hospice Programs
· Live in a nursing facility, swing bed, intermediate care facility for the mentally retarded, the State Hospital, or Anne Carlsen School
Individuals who buy into Medicaid through the Workers with Disabilities or Children with Disabilities coverages pay a small premium.
Who is eligible?
Medicaid provides coverage to:
· Children in foster care or subsidized adoption
· Children with disabilities (birth to 19)
· Other children up to age 21
· Pregnant women
· Women with breast or cervical cancer
· Parents or caretakers of deprived children
· Workers with disabilities
· Other blind and disabled individuals
· Individuals age 65 or older
· Low-income Medicare beneficiaries (Medicare Savings Programs).
Most children under age 19 become continuously eligible for Medicaid. That is, once they are determined eligible, they stay eligible for up to 12 months without regard to changes in circumstances. Similarly, most pregnant women who become elegible remain eligible through their pregnancy and for at least 60 days after the preganancy ends.
Medicaid coverage may begin up to 3 calendar months prior to the month of application.
Individuals that are not covered by Medicaid are adults between the ages of 21 and 65 who are not blind or disabled, pregnant, or a caretaker of deprived children.
Medicaid provides coverage to:
Most children under age 19 become continuously eligible for Medicaid. That is, once they are determined eligible, they stay eligible for up to 12 months without regard to changes in circumstances. Similarly, most pregnant women who become eligible remain eligible through their pregnancy and for at least 60 days after the pregnancy ends.
Medicaid coverage may begin up to 3 calendar months prior to the month of application.
Medicaid Eligibility Requirements (starting January 2015)The following is a general outline of Medicaid Program eligibility requirements.
State ResidenceYou must be a state resident to qualify for Medicaid in North Dakota.
CitizenshipYou must be a United States citizen or an alien who is lawfully admitted for permanent residence. Some lawfully admitted aliens who were admitted to the United States after August 22, 1996, may have to wait for five years before full Medicaid benefits are available. After the five years, aliens who are lawfully admitted, who are credited with 40 qualifying quarters of social security coverage, may be eligible for Medicaid.
Note: Qualifying quarters for any quarter in which TANF, SNAP, Medicaid, or SSI benefits were received are not counted.
There is no waiting period for coverage of emergency services.
Asset LimitsThere is no asset limit for children, families, or pregnant women in the Children and Families coverage group, the Adult Expansion Group (individuals between the ages of 19 and 65), or the Women's Way program.
Generally, a person who is blind, disabled, or age 65 or older can have up to $3000 in countable assets (such as savings accounts, checking accounts, stocks, bonds, or other type of asset) to qualify for Medicaid. The limit for couples is $6000. For each additional person in the household, $25 can be added to the asset limits.
Individuals who qualify for the Workers with Disabilities coverage are allowed an additional $10,000.
Those requesting eligibility under the Medicare Savings Program have an asset limit of $7,280 for a one-person household or $10,930 for a two-person household.
Spousal Impoverishment Prevention Coverage - This coverage applies to couples where one needs Nursing Care Services in a facility or at
home.
The spouse receiving the nursing care services is allowed $3000. The spouse who remains in the community is entitled to keep half of the couple's countable assets, but not less than $23,844 and not more than $119,220 for calendar year 2015.
The spouse receiving the nursing care services may keep up to $65 of their monthly income and may deem income to bring the income of the spouse in community up to $2,267 per month and any dependent household members up to $655.
Assets that are not counted
Income - Depending on the amount of net income, individuals may be eligible for full Medicaid benefits or may be responsible for a portion of their medical bills which is called Client Share (Recipient Liability). Children who are not eligible for full Medicaid benefits may qualify for Healthy Steps.
Those who qualify under the new Adult Expansion group, families with children, and pregnant women are subject to MAGI (Modified Adjusted Gross Income) rules. MAGI rules differ from traditional Medicaid in that household size is based on tax filing status, and treatment of income is based on Modified Adjusted Gross Income.
The following expenses are allowed for those aged and disabled individuals subject to non-MAGI rules:
Individuals in a nursing home are allowed to keep $65 of their monthly income to meet their personal needs. They also keep enough to cover their health insurance premiums and certain other expenses. If the individual has a family at home with lower income, the individual can give some of his/her money to the family at home.
Individuals residing in an Intermediate Care Facility are allowed $100 to meet their personal needs. They also keep enough to cover their health insurance premiums and certain other expenses.
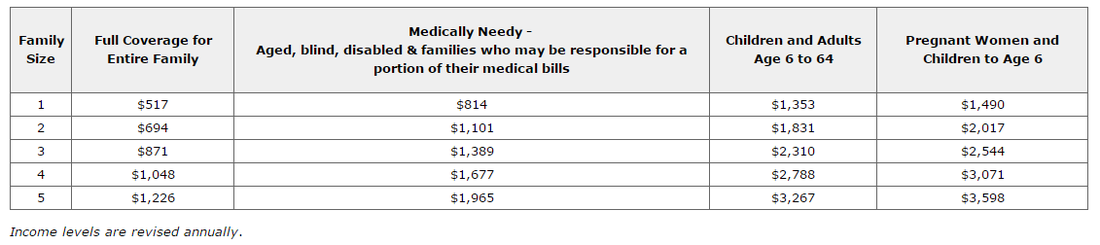
General Medicaid Income Levels
Effective April 1, 2015
Who can apply for programs or services?
Generally speaking, anyone may apply for assistance. Eligible applicants will ordinarily reside in North Dakota.
Where do I apply for programs and services?
To apply, contact your local County Social Service Office. For local contact information, click on the county closest to your home on the locator map. You may also view the Application for Assistance, complete it, print and sign it, and deliver it to the County Social Service Office. Completing the application prior to visiting the County Social Service Office may help to shorten the eligibility determination process. You can also complete and file the application electronically using the online application system.
Will there be any cost to me for programs or services?
Some people are required to pay co-payments for services received, and some may also be required to pay a recipient liability. Individuals DO NOT have to pay co-payments if they:
· Are younger than age 21
· Are pregnant
· Are tribal members enrolled in Medicaid and receiving services under a referral from Contract Health Services (CHS)
· Need emergency services
· Receive family planning services
· Receive Medicaid through the Women's Way or Medicaid Hospice Programs
· Live in a nursing facility, swing bed, intermediate care facility for the mentally retarded, the State Hospital, or Anne Carlsen School
Individuals who buy into Medicaid through the Workers with Disabilities or Children with Disabilities coverages pay a small premium.
Who is eligible?
Medicaid provides coverage to:
· Children in foster care or subsidized adoption
· Children with disabilities (birth to 19)
· Other children up to age 21
· Pregnant women
· Women with breast or cervical cancer
· Parents or caretakers of deprived children
· Workers with disabilities
· Other blind and disabled individuals
· Individuals age 65 or older
· Low-income Medicare beneficiaries (Medicare Savings Programs).
Most children under age 19 become continuously eligible for Medicaid. That is, once they are determined eligible, they stay eligible for up to 12 months without regard to changes in circumstances. Similarly, most pregnant women who become elegible remain eligible through their pregnancy and for at least 60 days after the preganancy ends.
Medicaid coverage may begin up to 3 calendar months prior to the month of application.
Individuals that are not covered by Medicaid are adults between the ages of 21 and 65 who are not blind or disabled, pregnant, or a caretaker of deprived children.
Medicaid provides coverage to:
- Low-income individuals from birth
- Children in foster care or subsidized adoption
- Former foster care children up to age 26, under certain circumstances
- Children with disabilities (birth to 19)
- Pregnant women
- Women with breast or cervical cancer
- Workers with disabilities
- Other blind and disabled individuals
- Low-income Medicare beneficiaries (Medicare Savings Programs)
Most children under age 19 become continuously eligible for Medicaid. That is, once they are determined eligible, they stay eligible for up to 12 months without regard to changes in circumstances. Similarly, most pregnant women who become eligible remain eligible through their pregnancy and for at least 60 days after the pregnancy ends.
Medicaid coverage may begin up to 3 calendar months prior to the month of application.
Medicaid Eligibility Requirements (starting January 2015)The following is a general outline of Medicaid Program eligibility requirements.
State ResidenceYou must be a state resident to qualify for Medicaid in North Dakota.
CitizenshipYou must be a United States citizen or an alien who is lawfully admitted for permanent residence. Some lawfully admitted aliens who were admitted to the United States after August 22, 1996, may have to wait for five years before full Medicaid benefits are available. After the five years, aliens who are lawfully admitted, who are credited with 40 qualifying quarters of social security coverage, may be eligible for Medicaid.
Note: Qualifying quarters for any quarter in which TANF, SNAP, Medicaid, or SSI benefits were received are not counted.
There is no waiting period for coverage of emergency services.
Asset LimitsThere is no asset limit for children, families, or pregnant women in the Children and Families coverage group, the Adult Expansion Group (individuals between the ages of 19 and 65), or the Women's Way program.
Generally, a person who is blind, disabled, or age 65 or older can have up to $3000 in countable assets (such as savings accounts, checking accounts, stocks, bonds, or other type of asset) to qualify for Medicaid. The limit for couples is $6000. For each additional person in the household, $25 can be added to the asset limits.
Individuals who qualify for the Workers with Disabilities coverage are allowed an additional $10,000.
Those requesting eligibility under the Medicare Savings Program have an asset limit of $7,280 for a one-person household or $10,930 for a two-person household.
Spousal Impoverishment Prevention Coverage - This coverage applies to couples where one needs Nursing Care Services in a facility or at
home.
The spouse receiving the nursing care services is allowed $3000. The spouse who remains in the community is entitled to keep half of the couple's countable assets, but not less than $23,844 and not more than $119,220 for calendar year 2015.
The spouse receiving the nursing care services may keep up to $65 of their monthly income and may deem income to bring the income of the spouse in community up to $2,267 per month and any dependent household members up to $655.
Assets that are not counted
- Your home
- One automobile
- Burial plans (with limits)
- Self-employment property (including tools, equipment and livestock)
- Non-saleable property, personal effects and clothing, household goods, and furniture
- Indian trust and restricted lands and per capita and judgment funds.
- Other miscellaneous assets
Income - Depending on the amount of net income, individuals may be eligible for full Medicaid benefits or may be responsible for a portion of their medical bills which is called Client Share (Recipient Liability). Children who are not eligible for full Medicaid benefits may qualify for Healthy Steps.
Those who qualify under the new Adult Expansion group, families with children, and pregnant women are subject to MAGI (Modified Adjusted Gross Income) rules. MAGI rules differ from traditional Medicaid in that household size is based on tax filing status, and treatment of income is based on Modified Adjusted Gross Income.
The following expenses are allowed for those aged and disabled individuals subject to non-MAGI rules:
- Taxes and other work related expenses
- Health insurance premiums
- Dependent care expenses
- Child support paid to a non-household member
- Other deductions may apply
Individuals in a nursing home are allowed to keep $65 of their monthly income to meet their personal needs. They also keep enough to cover their health insurance premiums and certain other expenses. If the individual has a family at home with lower income, the individual can give some of his/her money to the family at home.
Individuals residing in an Intermediate Care Facility are allowed $100 to meet their personal needs. They also keep enough to cover their health insurance premiums and certain other expenses.
General Medicaid Income Levels
Effective April 1, 2015
SOURCE: https://www.nd.gov/dhs/services/medicalserv/medicaid/eligible.html
What do I do if my child doesn’t qualify for Medicaid?
Do you know a child who doesn't have health insurance coverage? The state's Healthy Steps Children's Health Insurance Program (SCHIP) can provide a healthier future for many of these children.
Healthy Steps insurance is for children who:
· do not have health insurance coverage
· are 18 years of age or younger
· do not qualify for the North Dakota Medicaid Program
· live in families with qualifying incomes
What is SCHIP?
The State Children's Health Insurance Program, or SCHIP, was established by the federal government ten years ago to provide health insurance to children in families at or below 200 percent of the federal poverty line.
To find out more about the North Dakota State CHIP Program click here. By visiting this site you will see North Dakota specific information about covered services, who is eligible, how to apply, copayments, frequently ask questions, and more!
For SCHIP assistance:
Phone: 1-877-KIDSNOW (1-877-543-7669)
ND Relay TTY: (800) 366-6888 or 711
SOURCE: North Dakota Department of Human Service
What do I do if my child doesn’t qualify for Medicaid?
Do you know a child who doesn't have health insurance coverage? The state's Healthy Steps Children's Health Insurance Program (SCHIP) can provide a healthier future for many of these children.
Healthy Steps insurance is for children who:
· do not have health insurance coverage
· are 18 years of age or younger
· do not qualify for the North Dakota Medicaid Program
· live in families with qualifying incomes
What is SCHIP?
The State Children's Health Insurance Program, or SCHIP, was established by the federal government ten years ago to provide health insurance to children in families at or below 200 percent of the federal poverty line.
To find out more about the North Dakota State CHIP Program click here. By visiting this site you will see North Dakota specific information about covered services, who is eligible, how to apply, copayments, frequently ask questions, and more!
For SCHIP assistance:
Phone: 1-877-KIDSNOW (1-877-543-7669)
ND Relay TTY: (800) 366-6888 or 711
SOURCE: North Dakota Department of Human Service